What Causes Chronic Fatigue Syndrome?
What is Chronic Fatigue Syndrome?
Chronic fatigue syndrome (CFS), also referred to as myalgic encephalomyelitis, is a multi-systemic and complex illness characterised by persistent and disabling fatigue that is not relieved with rest and is associated with physical and cognitive symptoms. [1,2]
Chronic Fatigue Syndrome Symptoms
The most common symptoms of chronic fatigue syndrome include exhaustion, tiredness, feeling drained of energy, heaviness in the limbs, muscle aches and pains, and brain fog. [1,3]
Patients often report significant impairments in cognition and concentration, including reduced processing speed of information, impaired memory and attention, mood changes and feeling unrefreshed due to interrupted sleep. [1,4,5]
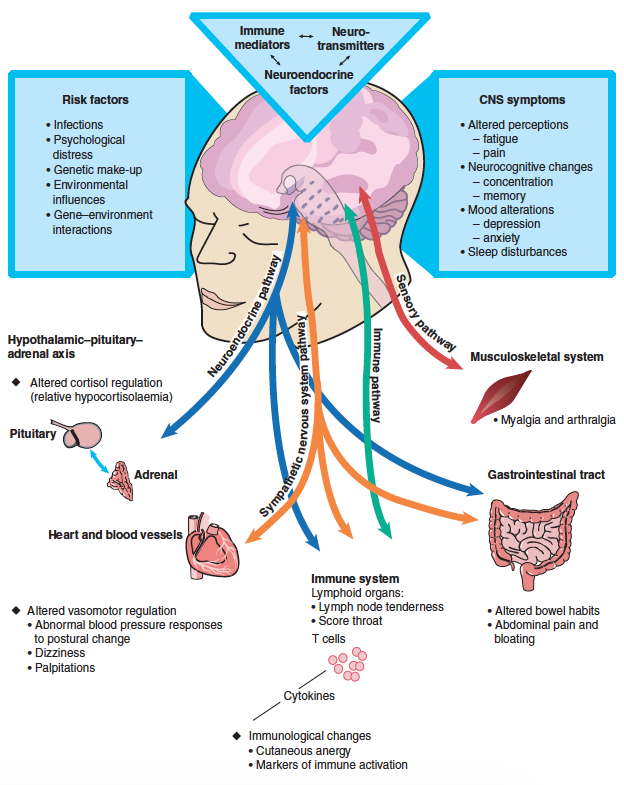
The overlapping nature of chronic fatigue syndrome
Source: Royal Australasian College of Physicians. Chronic Fatigue Syndrome. Clinical Practice Guidelines-2002.
Studies using positron emission tomography (PET), and whole-brain magnetic resonance spectroscopy have found evidence of widespread neuroinflammation in the brains of chronic fatigue patients. [2]
Neuro-inflammation, which is linked to neurocognitive impairment and neurodegenerative disorders, is a common feature in chronic fatigue syndrome, affects 85% to 90% of all patients. [2]
Other common symptoms include enlarged lymph nodes, headaches, fibromyalgia, irritable bowel syndrome, and postural orthostatic tachycardia syndrome. [3,5]
Chronic fatigue syndrome also presents with a characteristic pattern of prolonged malaise, and muscle aches and pains following activity, exercise or activity that does not improve after rest. [1,6]
Patients with chronic fatigue syndrome frequently experience mood disturbances, including major depression, and frequently fail to respond well to antidepressant medications, unless the patient is presenting with features of comorbid depression. [7]
Causes of Chronic Fatigue Syndrome
First described in the mid-1980s, little was known about the underlying causes of Myalgic Encephalomyelitis or Chronic Fatigue Syndrome. [4]
Thousands of investigations over the last 35 years, however, have identified abnormalities involving many organ systems in patients with chronic fatigue syndrome. [4]
It has been demonstrated that chronic fatigue syndrome might be due to multiple factors, which is particularly complex. This includes:
Source: Royal Australasian College of Physicians. Chronic Fatigue Syndrome. Clinical Practice Guidelines-2002.
THE CENTRAL AND AUTONOMIC NERVOUS SYSTEM - Abnormalities in the autonomic nervous system have been repeatedly demonstrated in chronic fatigue syndrome. [6]
Multiple studies have found central and autonomic nervous system dysfunction, involving the impairment in the function of the limbic-hypothalamic-pituitary-adrenal axis, which is responsible for mood and hormone regulation. [4]
PSYCHOLOGICAL OR PSYCHOSOCIAL FACTORS - There is a strong relationship between chronic fatigue syndrome and psychological disorders. [8,9,10]
Psychosocial causes of fatigue, such as depression and anxiety have been shown to be the most common non-somatic diagnoses. [11]
There is strong evidence to suggest that childhood trauma increases the risk of chronic fatigue syndrome. [12]
IMMUNOLOGIC FACTORS - Common, non-specific viral illnesses are unlikely to cause the onset of chronic fatigue syndrome. Specific infections, such as enteroviruses, retroviruses, and infectious mononucleosis, also known as glandular fever, which is caused by the Epstein–Barr virus (EBV), have all been linked to the development of chronic fatigue syndrome. [3,5]
It appears that Ross River virus and non-viral infections like (Q fever, Lyme disease, and Mycoplasma have also been linked to chronic fatigue syndrome, [3,5] and Epstein–Barr virus has been shown to be a risk factor in the cause of multiple sclerosis. [2]
METABOLIC CHANGES - The mitochondria are extremely sensitive to psychological and physical stressors, which can result in a reduction in overall energy production. [1,4]
Chronic fatigue syndrome may be linked to a decline in mitochondrial function as a result of free radical production and oxidative stress. [1,4]
FOOD AND ENVIRONMENTAL INTOLERANCES - Though not considered a direct cause of chronic fatigue syndrome, patients frequently have food intolerances that can aggravate symptoms, as a link has been found between multiple chemical sensitivities, sick building syndrome and chronic fatigue syndrome. [5]
How to Diagnose Chronic Fatigue Syndrome
Diagnosing chronic fatigue syndrome requires a complete evaluation of your medical history and mental health as well as a thorough physical examination, which includes the appropriate investigations to rule out any suspected medical conditions. [5]
Since there is no single medical diagnostic test or well-defined pathophysiology for chronic fatigue syndrome, medical practitioners may delay diagnosing it or misdiagnose it due to normal laboratory results. [13]
In adults, the most common disorders associated with chronic fatigue syndrome include sleep apnoea, hypothyroidism, anaemia, coeliac disease, chronic hepatitis, panic disorder, generalised anxiety, major depression, and somatoform disorders. [5]
Treating Chronic Fatigue Syndrome
If you have been diagnosed with chronic fatigue syndrome, a single treatment is very unlikely to result in a "cure," and switching from one form of treatment to another in search of a “quick fix” or “cure" should be avoided, as it is likely to result in frustration with a significant impact on your long-term outcomes. [5]
Due to the overlapping nature of chronic fatigue syndrome, treatment requires a continuous, multidisciplinary, cooperative person-centred approach to meet your unique needs and improve your quality of life.
This may be a reason that many patients with chronic conditions seek additional care outside mainstream medicine, often consulting complementary medicine practitioners, such as naturopathic practitioners, chiropractors, osteopaths, nutritionists, and acupuncturists. [14]
The naturopathic treatment process often incorporates an integrative medicine approach, which includes a variety of nutritional and herbal medicines, as well as dietary, lifestyle, and patient education that is tailored to the patient’s specific circumstances. [14]
It has been shown that doctors who are proactive in providing accurate information and discussing critical issues with their patients on a regular basis are more likely to achieve the best outcomes. [5]
Naturopathic medicine practitioners tend to provide longer consultations compared to medical doctors, which allows the opportunity for the naturopathic practitioner to engage with the patient and explore the patient’s complex, multifactorial needs. [14]
This person-centred care or personalised approach has been demonstrated to improve patients' sense of self-efficacy and empowerment, as well as contribute to feeling heard and supported. [14]
From a naturopathic, integrative, and functional medicine perspective, the goal in treating chronic fatigue syndrome is to make steady progress towards improving your functional capacity, which is rarely achieved without some degree of setback, exacerbation, or fluctuation in your symptoms during the process. The treatment goals may include addressing the following:
Stress management counselling - how to cope with the stress?
Central and autonomic nervous system function, including limbic-hypothalamic-pituitary-adrenal axis dysfunction
Immunological factors, such as treating bacterial and viral infections, food and environmental intolerance
Multiple chemical sensitivities and toxic metal overload
Neuro-Inflammation and oxidative stress
Gut-Brain axis and the microbiome
Are You Struggling With Chronic Fatigue? Request a Call Back to learn more.
DR ALAIN FRABOTTA is a highly qualified and experienced integrative chiropractor and functional medicine naturopathic doctor in Sydney since 1995.
With a specific interest in the treatment, prevention, and management of complex chronic diseases, including stress management and mental health.
Alain provides a holistic, person-centred, multidisciplinary, solution-focused, results-driven approach.
He integrates chiropractic, naturopathic and functional medicine, nutrition, counselling, and coaching to help you bridge the gap between your physical, mental, and spiritual health.
Alain is the leading integrative chiropractic and functional medicine naturopathic doctor in Sydney who wants to help you achieve your health and well-being goals as well as reach your full potential in life.
He is also dedicated to providing you with a personalised, targeted treatment approach that employs functional and genomic assessments to diagnose and optimise your health, well-being, and performance.
Learn more about DR ALAIN FRABOTTA
Managing Stress and Fatigue
The use of mind-body approaches to improve the relationship between your brain, mind, and body, and behaviour to strengthen self-awareness and self-care. This can help to improve your mood, ability to cope, and quality of life. [15]
There is evidence to suggest that rehabilitative, behavioural and cognitive approaches can help to identify limiting beliefs, attitudes and behaviours that can be of benefit in resolving chronic fatigue syndrome. [5]
Such treatments are not designed to provide immediate relief of symptoms. Rather, they aim to overcome potential obstacles to recovery and maximise functional capacity while developing coping strategies over a longer period of time. [5]
This includes assisting patients in recovering from traumatic stress, which provides evidence-based practical strategies and tools to help heal the past, build resilience and live in the present.
Patients who incorporate a behavioural and cognitive component in their treatment are more likely to maintain short and long-term improvements. [5]
This could be due to the ease with which they gain a better understanding of their illness, avoid potentially harmful treatments, implement appropriate management strategies, develop practical coping skills, and adopt lifestyle changes. [5]
Sleep Management - There is an association that an imbalanced circadian rhythm could contribute to chronic fatigue syndrome. There is a growing acceptance that restoring the sleep-wake cycle and circadian rhythm should play be an important goal in the treatment of patients with chronic fatigue syndrome. [5,16]
Chronic Fatigue Syndrome and Nutrition
The quality of evidence-based nutritional intervention for chronic fatigue syndrome has significantly grown. [1]
The mitochondria appear to contribute to the complex pattern of symptoms in chronic fatigue syndrome, as cellular mitochondrial damage can impact the cell's abilities to produce energy and produce symptoms of fatigue. [1]
Nutrition interventions may help to mitigate the risks associated with free radical damage often present in chronic fatigue patients. [1]
Free radical damage or stimulation of the immune-inflammatory, nitrosative and oxidative stress responses, often present in chronic fatigue patients have been shown to promote brain disorders, such as brain hypoperfusion/hypometabolism, neuro-inflammation, DNA damage, mitochondrial dysfunction, and secondary autoimmune conditions. [1]
Chronic Fatigue Syndrome and Medicinal Plants
Medicinal plants preparations, often known as botanical and herbal medicines are made up of many chemical constituents rather than a single compound.
There is sufficient traditional, empirical, and clinical evidence that botanical medicines provide anti-viral, anti-inflammatory and immune-modulating properties, while also helping to increase your adaptability, resilience, and alleviate stress. [17,18]
Medicinal plants continue to provide the basic raw material for some of the most important antiviral drugs. [17]
Despite the development of new antiviral drugs derived from synthetic sources, these drugs are responsible for many harmful effects. [17]
What Next? Read: 8 Steps To Optimum Health and Well-Being
Please feel free to reach out if you have any questions or feedback
+ REFERENCES
[1] Bjørklund G, Dadar M, Pen JJ, Chirumbolo S, Aaseth J. Chronic fatigue syndrome (CFS): Suggestions for a nutritional treatment in the therapeutic approach. Biomed Pharmacother. 2019;109:1000-1007. doi:10.1016/j.biopha.2018.10.076
[2] Williams PhD MV, Cox B, Lafuse PhD WP, Ariza ME. Epstein-Barr Virus dUTPase Induces Neuroinflammatory Mediators: Implications for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Clinical Therapeutics. 2019;41(5):848-863. doi:10.1016/j.clinthera.2019.04.009
[3] Sandler CX, Hamilton BA, Horsfield SL, et al. Outcomes and predictors of response from an optimised, multidisciplinary intervention for chronic fatigue states. Internal Medicine Journal. 2016;46(12):1421-1429. doi:10.1111/imj.13251
[4] Komaroff AL. Advances in Understanding the Pathophysiology of Chronic Fatigue Syndrome. JAMA. 2019;322(6):499. doi:10.1001/jama.2019.8312
[5] Working Group of the Royal Australasian College of Physicians. Chronic fatigue syndrome. Clinical practice guidelines--2002. Med J Aust. 2002;176(S9):S17-S55.
[6] Keech A, Sandler CX, Vollmer-Conna U, Cvejic E, Lloyd AR, Barry BK. Capturing the post-exertional exacerbation of fatigue following physical and cognitive challenge in patients with chronic fatigue syndrome. J Psychosom Res. 2015;79(6):537-549. doi:10.1016/j.jpsychores.2015.08.008
[7] Griffith JP, Zarrouf FA. A systematic review of chronic fatigue syndrome: don't assume it's depression. Prim Care Companion J Clin Psychiatry. 2008;10(2):120-128. doi:10.4088/pcc.v10n0206
[8] Hickie IB, Hooker AW, Bennett BK, Hadzi‐Pavlovic D, Wilson AJ, Lloyd AR. Fatigue in selected primary care settings: sociodemographic and psychiatric correlates. Medical Journal of Australia. 1996;164(10):585-588. doi:10.5694/j.1326-5377.1996.tb122199.x
[9] Ridsdale L, Evans A, Jerrett W, Mandalia S, Osler K, Vora H. Patients with fatigue in general practice: a prospective study. BMJ 1993;307:103–06.
[10] Ridsdale L, Evans A, Jerrett W, Mandalia S, Osler K, Vora H. Patients who consult with tiredness: frequency of consultation, perceived causes of tiredness and its association with psychological distress. Br J Gen Pract 1994;44:413–16.
[11] Elnicki DM, Shockcor WT, Brick JE, Beynon D. Evaluating the complaint of fatigue in primary care: diagnoses and outcomes. Am J Med 1992;93:303–06.
[12] Heim C, Nater UM, Maloney E, Boneva R, Jones JF, Reeves WC. Childhood trauma and risk for chronic fatigue syndrome: association with neuroendocrine dysfunction. Arch Gen Psychiatry. 2009;66(1):72-80.
[13] Sandler CX, Lloyd AR. Chronic fatigue syndrome: progress and possibilities. The Medical Journal of Australia. 2020;212(9):428-433. doi:10.5694/mja2.50553
[14] Foley H, Steel A, Adams J. Perceptions of person-centred care amongst individuals with chronic conditions who consult complementary medicine practitioners. Complementary Therapies in Medicine. 2020;52:102518. doi:10.1016/j.ctim.2020.102518
[15] Khanpour Ardestani S, Karkhaneh M, Stein E, et al. Systematic Review of Mind-Body Interventions to Treat Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Medicina. 2021;57(7):652. doi:10.3390/medicina57070652
[16] van Heukelom RO, Prins JB, Smits MG, Bleijenberg G. Influence of melatonin on fatigue severity in patients with chronic fatigue syndrome and late melatonin secretion. Eur J Neurol. 2006;13(1):55-60
[17] Akram M, Tahir IM, Shah SMA, et al. Antiviral potential of medicinal plants against HIV, HSV, influenza, hepatitis, and coxsackievirus: A systematic review. Phytotherapy Research. 2018;32(5):811-822. doi:10.1002/ptr.6024
[18] Brendler T, Al‐Harrasi A, Bauer R, et al. Botanical drugs and supplements affecting the immune response in the time of COVID ‐19: Implications for research and clinical practice. Phytotherapy Research. Published online December 29, 2020. doi:10.1002/ptr.7008